QPP Reporting for Hospitals & Health Systems
Hospitals and Health Systems face especially unique challenges when navigating these requirements. The reimbursement of Medicare Part B services depends directly on the performance of each eligible department, clinic, and clinician. Accessing multiple Electronic Medical Records or billing software to get the right data from the right providers is another challenge, but crucial to successful reporting. Hospitals must also critically assess reporting options, determine clinician eligibility, and make the decision about whether to report as an individual or as a group, as these factors will impact the ease of reporting and overall reimbursement.
With our years of experience and a registry that has seen it all, we can assist in optimizing this process. You can rest assured that you are maximizing your QPP scores with proven data integrations and best-in-class calculation engines. And your organization can get back to focusing on patient care.

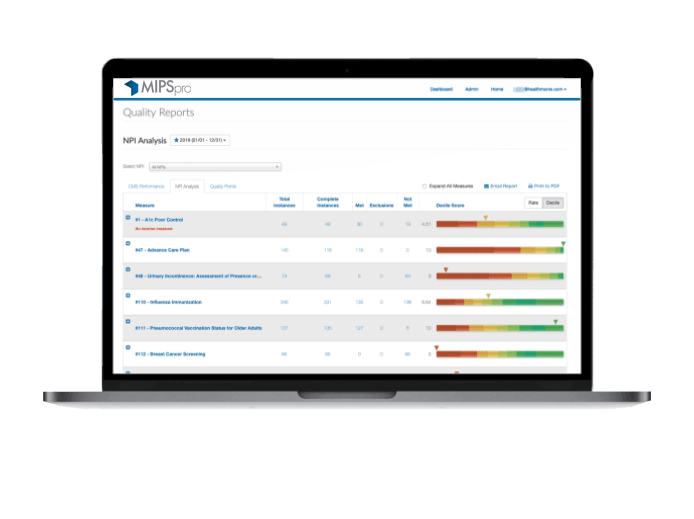
REAL-TIME MIPS UPDATES
Live performance updates allow timely decisions to close gaps in care. Our measure, patient, and provider dashboards support targeted improvement.
ALL MIPS CATEGORIES
MIPSpro is the only registry that tracks Quality, PI, IA, and Cost.

SUBMISSION VALIDATION
Our experts review each submission for costly mistakes based on the latest rulings from CMS. Our proprietary engine provides seamless, optimized submission and scoring.
US-BASED SUPPORT
Get quick, easy to understand answers to all of your MIPS questions from our expert, highly-rated support team.

YEAR-ROUND REPORTING
Quality measures are available during each performance year for year-round reporting. Our proprietary algorithm selects measures to target and report for the optimal score.

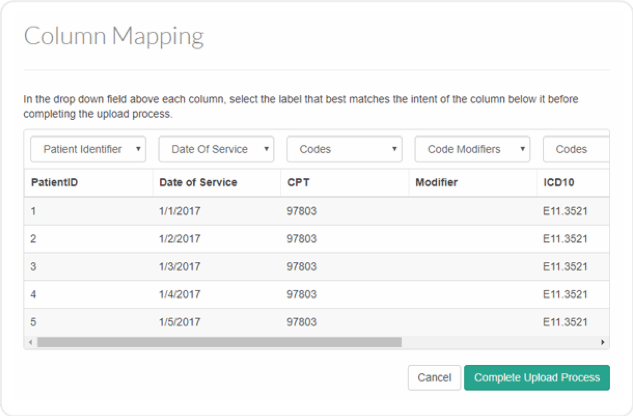
INTEGRATED DATA
Reporting from one or multiple EMRs is easy through flexible data integration options. No manual entry is required.
Multiple EHRs? No problem!
Healthmonix has provided streamlined reporting options as a CMS Qualified Registry since 2009. From solo providers to large Health Systems, we provide unmatched support and adaptable reporting plans to meet your goals. In 2017, we successfully submitted data from over 30 million patient visits and 233 different EHRs, leading to a 98.6% Customer Satisfaction Rating for our MIPSpro® Registry. Our platform, ACO PRO, allows Accountable Care Organizations to track and report 15 CMS Web Interface (WI) quality measures.
Comprehensive data integration
- Our clinical coding experts have integrated automatic translation of SNOMED, LOINC, RxNorm, NDC, CVX and other coding standards for cases where CMS numerator codes are not used by your EHR. This could save your staff hundreds of hours of work!
- Patient vitals and other clinical data are automatically accepted to meet numerator criteria for select measures. No translations into CMS codes needed!
- MIPSpro integrates data from multiple sources, an ideal feature for health systems that use multiple EHRs. We combine data to reveal areas for improvement, and to help you report the best measures for your organization.
Intelligent MIPS reporting
powered by the unique MIPSpro scoring engine.
- Select and track all measures for no extra cost, and select your top measures at submission.
- Streamlined policy compliance feedback ensures that thresholds are met.
- Smart scoring dashboards show actual vs. predicted scores and update in real-time.
- Submit BOTH group and individual level to get credit for whichever score is higher - at no extra cost.
- All clinical and claims data is mined to show best measures to report and areas for improvement
- Email Quality performance reports for your whole practice with one click.
Should you opt for Facility-Based scoring?
Hospitals and Health Systems should also consider the pros and cons of facility-based measurement, a participation option launched by CMS in their 2019 MACRA final rule that offers certain groups of facility-based clinicians the option to be scored based on their hospital’s overall performance. If these clinicians additionally decide to report MIPS quality measures in the standard way, CMS will award them the higher of the two scores.
Under facility-based measurement, individual clinicians can avoid reporting their own Quality measures but have no control over what measures and score they will ultimately receive, and less influence over facility-level performance improvement. Clinicians focused on MIPS incentive maximization should therefore choose a reporting mechanism that better enables performance improvement, like a Qualified Registry or QCDR.