Audiology MIPS Reporting in 2022
Learn more about important MIPS 2022 updates

Step 1: Discover if you're MIPS-eligible
Since 2019, the pool of eligible clinicians has expanded to include some of the previously excluded professions, including Physical / Occupational Therapists, Speech-Language Pathologists, Audiologists, Clinical Psychologists and Dietitians/Nutritional Professionals in MIPS reporting . Read More About Eligibility
In addition, clinicians participating in an APM that do not meet certain thresholds still need to participate in MIPS. Eligible clinicians under an APM entity that is both an Advanced and MIPS APM that are not QPs or Partial Qualifying APM Participants (Partial QPs), are scored under the APM Scoring Standard and do not need to participate in MIPS. However, note that the thresholds change each year and clinicians should check their status to ensure proper participation.
Eligible clinicians, groups, and APM entities are also able to elect to opt-in to MIPS if they exceed one or two, but not all elements of the low-volume threshold. That means that these previously ineligible clinicians have the opportunity to participate in the QPP and earn a payment adjustment.
Step 2: Learn why reporting MIPS matters
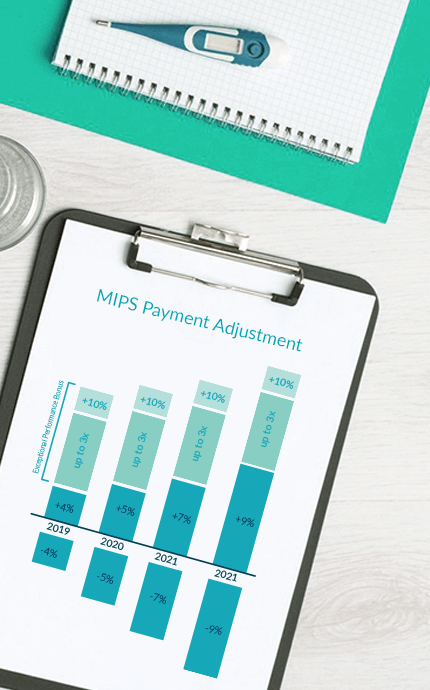
MIPS continues to move to more challenging performance metrics, resulting in larger incentives and penalties for those that participate. Historically, the incentives have been less than 2%, even for a ‘perfect’ score. That’s changing. The benchmark for avoiding a penalty continues to rise, and the ability to achieve that benchmark is tougher due to evolving regulations. This is resulting in the need to find an effective solution for MIPS reporting, sooner rather than later.
Unlike past quality initiatives, a clinician's MIPS payment adjustment will now follow them even after they depart from the TIN they reported under. In addition, the MIPS payment adjustment is used by other programs to adjust payments as well.
Physician Compare (now Care Compare): In addition to impacting eligible clinicians financially, MIPS performance has the potential to affect the reputation of eligible clinicians and groups. Scores are publicly posted as soon as the informal review period closes following the performance year.

Step 3 : Select your reporting goals
As the MIPS program matures, it’s important to thoughtfully set your goals each year. The options for 2021 are again more challenging compared to the options available for 2020 and the prior reporting years.
Attack your MIPS goals by understanding the 2022 updates!
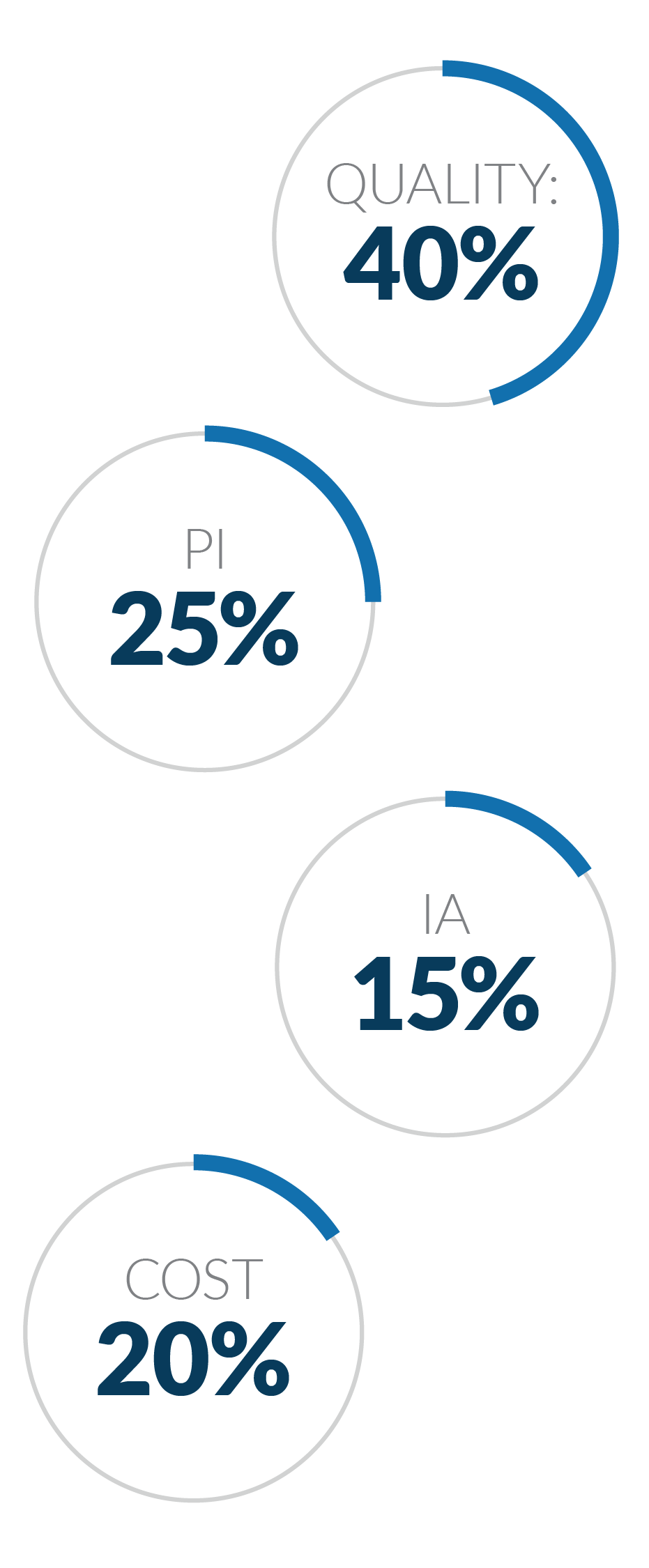
Step 4: Know the performance categories
Quality:
The MIPS Quality Performance Category is closely related to its predecessor, the Physician Quality Reporting System (PQRS). To successfully report Quality, participants must report six measures (one of which is an outcome measure) over a full calendar year for at least 70% of the applicable patient visits.
Promoting Interoperability:
The Promoting Interoperability (PI) Performance Category focuses on the use of 2015 CEHRT technology for e-prescribing, HIE, patient engagement, and public health and clinical data exchange. For 2020 and 2021, clinicians will submit a single set of PI measures to align with 2015 edition CEHRT. This single measure set includes slight changes for 2021. Some measures continue to be ‘yes/no’, while many are proportional and measure the number of eligible participants for which the measures have been completed.
* You will likely be exempt from reporting PI, but please confirm with CMS.
Improvement Activities:
The Improvement Activities Performance Category rewards eligible clinicians for participating in specified activities aimed at improving quality of care. Clinicians and groups can choose to participate in activities most relevant to both their practice and patient population. For groups, at least 50% of eligible clinicians need to participate in the improvement activities for at least 90 days during the year. Recommended Improvement Activities for the Audiology Clinical Registry include:
IA_EPA_2 - Use of telehealth services that expand practice access
IA_PM_15 - Implementation of episodic care management practice improvements
IA_BE_6 - Collection and follow-up on patient experience and satisfaction data on beneficiary engagement
IA_BE_15 - Engagement of Patients, Family, and Caregivers in Developing a Plan of Care
IA_PSPA_1 - Participation in an AHRQ-listed patient safety organization
IA_PSPA_19 - Implementation of formal quality improvement methods, practice changes, or other practice improvement processes
Cost:
The Cost Performance Category score is the average performance total for the Medicare Spending Per Beneficiary (MSPB) measure, the Total per Capita Cost measure, and 18 episode-based measures (when applicable). Cost is computed at a clinician group level, based on meeting minimum episode thresholds for each measure. All Cost measures are automatically captured through administrative claims.
* You will likely be exempt from Cost, but please confirm with CMS.
Step 5 : Report with Healthmonix's Audiology Clinical Registry
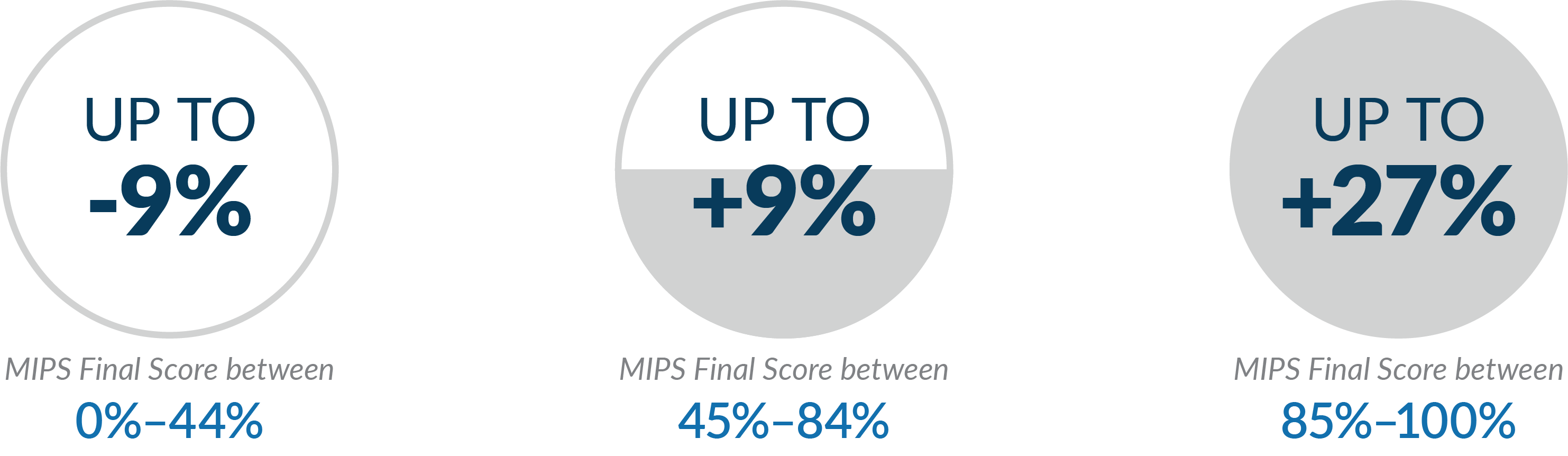
Under MIPS, performance matters! It's no longer enough to just report quality data. In 2022, CMS will issue a -9% penalty to organizations that receive a low final MIPS score, and high performers will be eligible for the 9% incentive and an exceptional performance bonus of up to 14%. Medicare quality reporting is complicated, but our Audiology Clinical Registry via MIPSpro® makes the reporting process easy. Our intuitive system and quality reporting team will guide you through the MIPS reporting process and to success!

THE AUDIOLOGY CLINICAL REGISTRY DELIVERS KEY FEATURES TO ENSURE YOUR SUCCESS:
- Real-time Dashboards
- MIPS Quality, PI, IA, and Cost for all specialties and all measures
- MIPSpro adapts to your practice
- Select reporting goals and track performance
- Integrated data
- Data Validation & Support
With prices starting as low as $289 per provider/year, starting today is the key to MIPS reporting success in 2022.