MIPS Value Pathways (MVPs)
Contact for pricing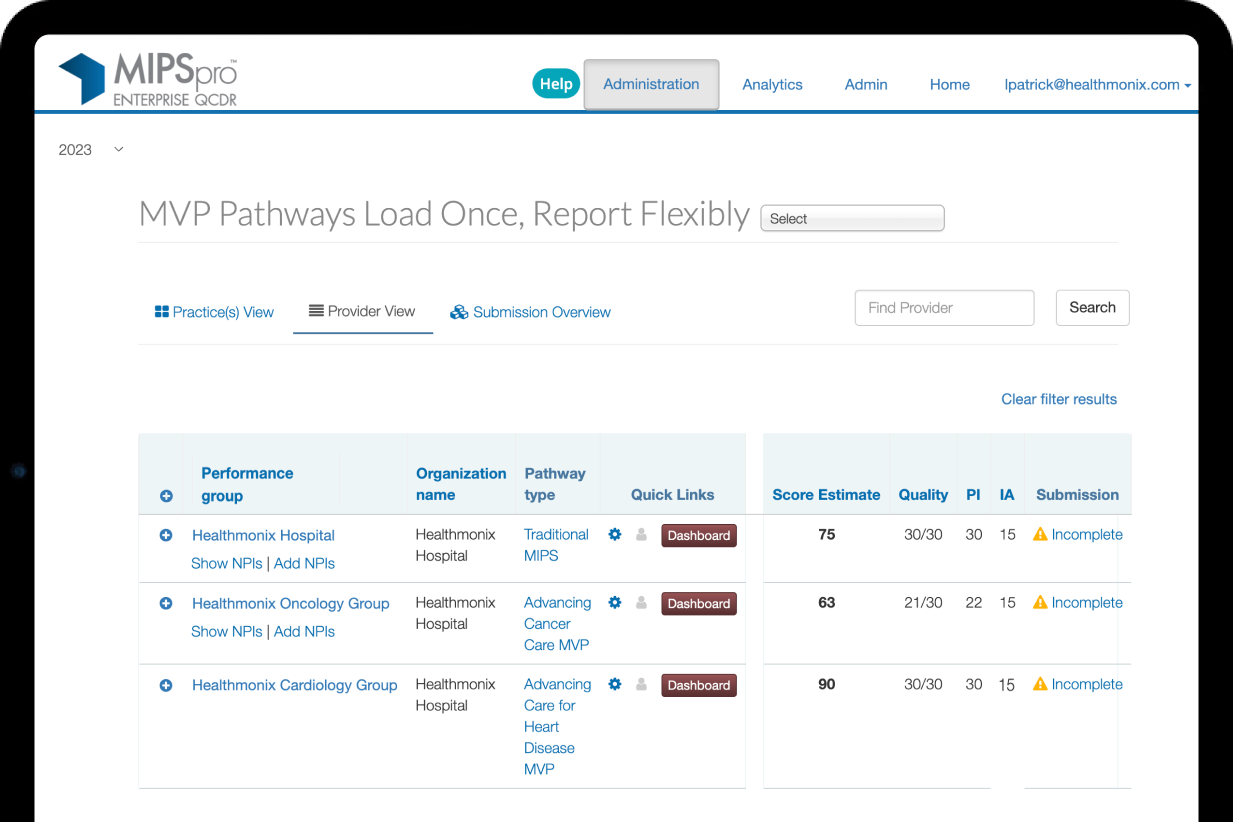
The next phase of MIPS reporting is here
MIPS Value Pathways are the newest reporting option to fulfill MIPS reporting requirements. The Centers for Medicare & Medicaid Services (CMS) created MVPs “to simplify MIPS clinician experience, improve value, reduce burden, and better inform patient choice in selecting clinicians.”
Each MVP is developed for a specialty or medical condition. MVPs offer more meaningful groupings of measures and activities, offering an improved assessment of quality of care (according to CMS).
Healthmonix supports all MVPs
Healthmonix will support all 16 MVPs available for the 2024 performance year. Our MIPSpro Qualified Registry and QCDR for MIPS Value Pathways (MVPs) optimizes your MIPS score and drives higher Medicare reimbursements by leveraging reporting pathways that are more relevant and produce more ROI to your specialty or practice.
Contact us to register with MIPSpro to track and report your MVP.
MVP registration requirements
CMS requires you to register for MVP participation through the QPP site, in addition to registering with our registry. To report an MVP, you’ll need to register through QPP for your MVP of choice, a population-health measure, and any outcomes-based claims measure needed. You’ll also need to register subgroups and the participants.

Dates of registration
MVP registration with CMS for the 2024 performance year runs April 1-Dec. 2, 2024. If you want to use the option to report the CAHPS for MIPS Survey as a measure in your MVP, you need to complete your MVP and CAHPS for MIPS Survey registrations before June 30, 2024.
The Quality Payment Program website features additional resources for understanding and implementing MVPs.

Available MVPs
CMS has approved 16 MVPs for the 2024 performance year. Click on an MVP name to see the measures and activities available to report within it.
- Adopting Best Practices and Promoting Patient Safety within Emergency Medicine
- Advancing Cancer Care
- Advancing Care for Heart Disease
- Advancing Rheumatology Patient Care
- Coordinating Stroke Care to Promote Prevention and Cultivate Positive Outcomes
- Focusing on Women’s Health
- Improving Care for Lower Extremity Joint Repair
- Optimal Care for Kidney Health
- Optimal Care for Patients with Episodic Neurological Conditions
- Patient Safety and Support of Positive Experiences with Anesthesia
- Prevention and Treatment of Infectious Disorders Including Hepatitis C and HIV
- Quality Care for the Treatment of Ear, Nose, and Throat Disorders
- Quality Care in Mental Health and Substance Use Disorders
- Rehabilitative Support for Musculoskeletal Care
- Supportive Care for Neurodegenerative Conditions
- Value In Primary Care
MVP reporting notes

Quality
- You must select 4 quality measures from your MVP and meet the case minimum (at least 20 denominator eligible instances) for each measure.
- At least 1 measure must be an outcome measure.
- If no outcome measures are available, you may report a high-priority measure.

Improvement Activities
You must report 1 of the following 3 options. This is a reduced requirement from traditional MIPS reporting:
- Two medium-weighted improvement activities from your MVP
- One high-weighted improvement activity from your MVP
- The IA_PCMH activity (participation in a certified or recognized patient-centered medical home or a comparable specialty practice)

Promoting Interoperability
- You must submit the required PI measures (the same as under traditional MIPS). Bonus points are available for reporting measures that aren’t required.
- If reporting as a subgroup, you’ll submit your affiliated group’s data for the PI performance category.
- Review your special statuses with the QPP Participation Status tool. You may be exempt from the PI performance category if you qualify for certain special statuses.

Cost
- You don’t submit any data for the Cost performance category. CMS uses Medicare claims data to calculate your cost measure performance.
- If you don’t meet the case minimum for any of the cost measures in your MVP, CMS will reweight the Cost performance category to 0%.

Foundational Layer — Population Health
- You must select 1 population-health measure at the time of MVP registration with CMS.
- You don’t submit any data for this measure. CMS will calculate the population-health measures for you using administrative claims data.
- This measure will be excluded from scoring if the measure doesn’t have a benchmark or meet the case minimum.