Introduction
This document details the methodology for the revised Medicare Spending Per Beneficiary (MSPB) clinician measure and should be reviewed along with the Measure Codes List file, which contains the medical codes used in constructing the measure.
Measure Description
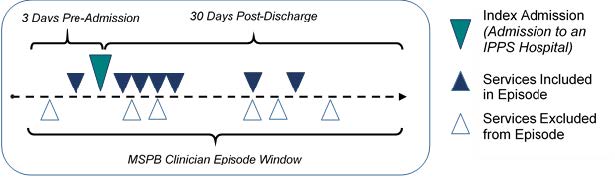
The revised MSPB clinician measure assesses the cost to Medicare of services provided to a beneficiary during a revised MSPB clinician episode (hereafter referred to as the “episode”), which comprises the period immediately prior to, during, and following the beneficiary’s hospital stay. An episode includes Medicare Part A and Part B claims with a start date between 3 days prior to a hospital admission (also known as the “index admission” for the episode) through 30 days after hospital discharge, excluding a defined list of services that are unlikely to be influenced by the clinician’s care decisions and are, thus, considered unrelated to the index admission. In all supplemental documentation, the term “cost” generally means the Medicare allowed amount, which includes both Medicare and trust fund payments and any applicable beneficiary deductible and coinsurance amounts Medicare spends on traditional, fee-for-service claims.
Rationale
Revised MSPB clinician is an important means of measuring Medicare spending, as health expenditures continue to increase in the United States. Total health care spending is estimated to have increased by 4.6 percent in 2017, reaching $3.5 trillion, and spending for Medicare, which is still predominantly paid on a fee-for-service (FFS) basis, grew by 3.6 percent, reaching $672.1 billion.2 In 2016, Medicare Fee-for-Service (FFS) paid $183 billion for approximately 10 million Medicare inpatient admissions and 200 million outpatient services, which reflects a 2.3 percent increase in hospital spending per FFS beneficiary between 2015 and 2016 (MedPAC, 2018). Given that the inpatient hospital setting is such an important contributor to overall Medicare spending, gauging the efficacy of this spending requires measuring the cost performance of clinicians providing care at hospitals. The revised MSPB clinician measure provides valuable context for such progress in efficiency by comparing the movement in costs associated with hospital admissions.
As background to this revised measure, a version of the revised MSPB clinician measure has been part of the Merit-based Incentive Payment System (MIPS) cost performance category since the 2017 MIPS performance period. Prior to this use in MIPS, CMS used the MSPB measure in the Value Modifier Program and reported it in annual Quality and Resource Use Reports (QRURs) until MACRA ended the Value Modifier Program. The current MSPB measure has undergone re-evaluation to address stakeholder feedback received from prior public comment periods. A technical expert panel (TEP) provided high-level guidance for the reevaluation of the measure at meetings in August 2017 and May 2018. The TEP consisted of 19 members from diverse backgrounds, including clinicians, healthcare providers, academia, and patient advocacy organizations. The TEP recommended the creation of a targeted MSPB Service Refinement Workgroup to provide detailed clinical input on service assignment rules.
The MSPB Service Refinement Workgroup comprised 25 clinicians representing a wide range of types of clinicians who may be attributed the revised MSPB clinician measure. The revised MSPB clinician measure underwent Field Testing in October 2018. A public comment period accompanied Field Testing, during which stakeholders reviewed and provided feedback on the Field Test Reports and the publicly posted supplementary documentation. Following Field Testing, the TEP reconvened in November 2018 to guide further measure refinement to address stakeholder feedback received through the public comment period.
Beneficiary Exclusion Criteria
Beneficiaries’ episodes are excluded from the measure population if they meet any of the following conditions:
- They were not enrolled in both Medicare Parts A and B for the entirety of the lookback period plus episode window.
- They were enrolled in a private Medicare health plan (e.g., a Medicare Advantage or a Medicare private FFS plan) for any part of the lookback period plus episode window.
- They resided outside the United States or its territories during any month of the measurement period.
Measure Numerator:
The numerator for the revised MSPB clinician measure is the sum of the ratio of payment-standardized observed to expected episode costs for all episodes attributed to the clinician group, as identified by a unique Medicare Taxpayer Identification Number (TIN), or to the clinician, as identified by a unique TIN and National Provider Identifier pair (TIN-NPI). The sum is then multiplied by the national average payment-standardized observed episode cost to generate a dollar figure.
Measure Denominator:
The denominator for the revised MSPB clinician measure is the total number of episodes attributed to a clinician or clinician group.
Data Sources
The revised MSPB clinician measure uses the following data sources:
- Medicare Parts A and B claims data from the Common Working File (CWF)
- Enrollment Data Base (EDB)
- Long Term Care Minimum Data Set (LTC MDS)
- Provider Enrollment, Chain and Ownership System (PECOS)
Care Settings:
The revised MSPB clinician cost measure can be triggered at acute care facility hospitals.
Quick Reference: Methodology Steps
There are two overarching processes in calculating revised MSPB clinician measure scores: episode construction (Steps 1-3) and measure calculation (Steps 4-6). This section provides a brief summary of these processes, and Section 4.0 describes them in detail.
- Define the population of index admissions: Episodes are opened, or triggered, by admission to an inpatient hospital. The episode window starts 3 days prior to this index admission and ends 30 days after discharge. Medicare Parts A and B claims billed during the episode window are considered for inclusion, and are refined as described in step 3.
- Attribute the episode to a clinician group: Episodes with medical Medicare Severity Diagnosis-Related Group (MS-DRGs) are attributed to any clinician group rendering at least 30 percent of evaluation and management (E&M) services on Medicare Part B Physician/Supplier claims during the index admission, and to any clinician who bills at least one E&M service that was used to determine the episode’s attribution to the clinician group. Episodes with surgical MS-DRGs are attributed to the clinician and clinician group rendering any main procedure determined to be clinically relevant to the index admission.
- Exclude unrelated services and calculate the episode observed cost: Clinically unrelated services are removed from the episode. The costs of the remaining services occurring during the episode window are summed to obtain each episode’s standardized observed cost.

- Exclude episodes: Exclusions remove a small, unique group of episodes from cost measure calculation in cases where it may be impractical and unfair to compare the costs of caring for these patients to the costs of caring for the cohort at large.
- Calculate expected episode cost through risk adjustment: Risk adjustment aims to isolate variation in clinician costs to only costs clinicians can reasonably influence (e.g., accounting for beneficiary age, comorbidities, and other factors). A regression model is applied to the risk adjustment variables to estimate the expected cost of each episode. Then, statistical techniques are applied to reduce the effect of extreme outliers on measure scores.
- Calculate the measure score: For each episode, the ratio of standardized observed cost (from step 3) to risk-adjusted expected cost (from step 5) is calculated and averaged across all of a clinician or clinician group’s attributed episodes to obtain the average episode cost ratio. The average episode cost ratio is multiplied by the national average observed episode cost to generate a dollar figure for the cost measure score.
Quick Reference: Specifications
This page provides a quick, at-a-glance reference for the revised MSPB clinician cost measure specifications. The full list of codes and logic used to define each component can be found within the Measure Codes List file.
| Episode Window: During what time period are costs measured? | |
| Pre-Index Admission Period: 3 days | Post-Discharge Period: 30 days |
| Triggers: Which patients are included in the measure? | |
| Admission to an inpatient hospital. The revised MSPB clinician cost measure can be triggered at acute care facility hospitals. | |
| Episode Attribution: How is revised MSPB clinician measure attributed at the TIN/TIN-NPI Levels? | |
The measurement period is a pre-defined and static calendar year performance period. Episodes ending during the measurement period are included in the calculation of the revised MSPB clinician measure. Episodes are attributed as follows: Episodes with Medical MS-DRGs Attributed to any clinician group rendering at least 30 percent of evaluation and management (E&M) services on Medicare Part B Physician/Supplier claims during the index admission, and to any clinician who bills at least one E&M service that was used to determine the episode’s attribution to the clinician group Episodes with Surgical MS-DRGs Attributed to the clinician and clinician group rendering any main procedure determined to be clinically relevant to the index admission | |
| Service Assignment: Which services are excluded from the measure? | |
Exclusions include a defined list of services that are unlikely to be influenced by the clinician’s care decisions. The service exclusion rules are defined specific to the Major Diagnostic Category (MDC) of the index admission. Service exclusions examples include:
| |
| Risk Adjustors: How does the measure adjust for beneficiary-level risk factors that can affect medical costs? | Exclusions: Which populations are excluded from the measure? |
|
|
Detailed Measure Calculation Methodology
Construction of revised MSPB clinician measure episodes is divided into three steps: (4.1) identifying index admissions, (4.2) attributing episodes to clinicians, and (4.3) calculating observed episode cost. Once measure episodes are constructed, measure calculation involves (4.4) creating comparable costs across episodes by excluding certain episodes, (4.5) estimating expected costs for the patient population based on patient comorbidities and other risk factors, and (4.6) calculating the average episode ratio and cost measure score. The following sections describe the six steps for calculating the revised MSPB clinician measure scores in more detail.
Define and Trigger Episodes
Episodes are opened, or triggered, by admissions to inpatient hospitals. The episode window is defined as the 3 days prior to this index admission to 30 days after the hospital discharge. There is a 90-day lookback period before the episode start date. This period is used to check beneficiary enrollment information for episode exclusions and beneficiary pre-existing health characteristics used for risk adjustment.
Attribute Episodes to Clinicians
Attribution is the process of determining which clinician groups are responsible for an episode. There are different methods of attribution depending on whether the MS-DRG is medical or surgical, with some exceptions.
The revised MSPB clinician measure utilizes two attribution methods for medical and surgical MS-DRG episodes. The measure attributes medical MS-DRG episodes to any clinician/clinician group that is responsible for managing the medical condition, and attributes surgical MS-DRG episodes to the clinician/clinician group performing the main procedure of an episode.
- For episodes in which the index admission has a medical MS-DRG, the episode is attributed first to the TIN that bills at least 30 percent of E&M codes found on Part B Physician/Supplier claims during the inpatient stay. The episode is then attributed to the TIN-NPI who billed at least one E&M service that was used to determine the episode’s attribution to the TIN.
- For episodes in which the index admission has a surgical MS-DRG, the episode is attributed to the TIN and TIN-NPI who billed any related surgical procedure on Part B Physician/Supplier claims during the inpatient stay. The full list of Current Procedural Terminology / Healthcare Common Procedure Coding System (CPT/HCPCS) codes determined as related to each surgical MS-DRG can be found in the Measure Codes List file.
Exclude Clinically Unrelated Services to Calculate Episode Observed Cost
Medicare Part A and Part B services during the episode window are considered for inclusion toward the episode, with exceptions for services that are unlikely to be influenced by the clinician’s care decisions. Clinically unrelated services are excluded based on service exclusion rules developed by the MSPB Service Refinement Workgroup. The service exclusion rules are defined specific to the Major Diagnostic Category (MDC) of the index admission. The service exclusion codes and logic for services deemed clinically unrelated can be found in the “SE_[General/Post]_Service_Category” tabs of the Measure Codes List file. The sum of the cost of the services that are included towards the episode is referred to as the episode observed cost.
Exclude Episodes
Before measure calculation can occur, a series of episode exclusions are applied to remove certain episodes from measure score calculation. Episodes are excluded from the revised MSPB clinician measure if they meet any of the following conditions:
- The beneficiary was not continuously enrolled in both Medicare Parts A and B from 90 days before episode start date through 30 days after discharge.
- The beneficiary’s death occurred during the episode.
- The beneficiary is enrolled in a Medicare Advantage plan or Medicare is the secondary payer at any time during the episode window or 90-day lookback period.
- The index admission for the episode did not occur in neither a subsection (d) hospital paid under the Inpatient Prospective Payment System (IPPS) nor in an acute hospital in Maryland.
- The discharge of the index admission occurred in the last 30 days of the measurement period.
- The index admission for the episode is involved in an acute-to-acute hospital transfer (i.e., the admission ends in a hospital transfer or begins because of a hospital transfer).
- The index admission inpatient claim indicates a $0 actual payment or a $0 standardized payment.
After applying the exclusions outlined above, all remaining episodes are included in the calculation of the revised MSPB clinician measure score.
Calculate Expected Episode Costs Through Risk Adjustment
Risk adjustment is used to estimate episode expected costs in recognition of the different levels of care beneficiaries may require due to comorbidities, disability, age, and other risk factors. A separate risk adjustment model is estimated for episodes within each MDC, which is determined by the MS-DRG of the index admission. This model includes variables from the CMS Hierarchical Condition Category Version 22 (CMS-HCC V22) 2016 Risk Adjustment Model and other standard risk adjustors to capture beneficiary characteristics.
Further detail about the revised MSPB clinician risk adjustment model is provided below:
- The model includes 12 age categorical variables, representing various age brackets.
- Severity of illness is measured using the MS-DRG of the index hospitalization, an indicator for any prior acute hospital admission, and 79 Hierarchical Condition Category (HCC) indicators with information derived from the beneficiary’s claims.
- The model includes status indicator variables for whether the beneficiary qualifies for Medicare through disability or age, End-Stage Renal Disease (ESRD), and whether the beneficiary is receiving long-term care (LTI).
- In addition, the model accounts for interactions between particular variables. Interaction terms are included because the presence of certain patient characteristics can increase expected cost in a greater way than predicted by the indicators alone.
- Patient characteristics are identified using Medicare Parts A and B claims that end in the 90-day lookback period from the episode start date.
Steps for defining risk adjustment variables and estimating the risk adjustment model are as follows:
- Define HCC and patient characteristic-related risk adjustors using Medicare Parts A and B claims in the 90-day lookback period from the episode start date.
- Define other risk adjustors that rely upon Medicare beneficiary enrollment and assessment data as follows:
- Identify beneficiaries who are originally “Disabled without end-stage renal disease (ESRD)” or “Disabled with ESRD” using the original reason for joining Medicare field in the Medicare beneficiary enrollment database.
- Identify beneficiaries with ESRD if their enrollment indicates ESRD coverage, ESRD dialysis, or kidney transplant in the Medicare beneficiary enrollment database in the 90-day lookback period.
- Identify beneficiaries who reside in a long-term care institution as of the episode trigger day using MDS assessment data.
- Drop risk adjustors that are defined for less than 15 episodes nationally for each MDC group to avoid using very small samples.
- Categorize beneficiaries into age ranges using their date of birth information in the Medicare beneficiary enrollment database. If an age range has a cell count less than 15, collapse this with the next adjacent age range category.
- Calculate an ordinary least squares (OLS) regression model to estimate the relationship between all the risk adjustment variables and the dependent variable, the standardized observed episode cost, to obtain the expected episode cost. A separate OLS regression is run for each episode MDC group nationally.
- Winsorize the expected episode cost by assigning the value of expected episode cost at the 0.5th percentile of the distribution for episodes within the same MDC to all episodes with expected episode costs below the 0.5th percentile.
- Renormalize values by multiplying each episode’s winsorized expected cost by the ratio of the MDC group’s average observed cost and the MDC group’s average winsorized expected cost.
- Exclude episodes with outlier residuals to obtain finalized expected episode cost. This step is performed across all episodes regardless of the MDC group.
- Calculate each episode’s residual as the difference between the observed cost and the re-normalized, winsorized expected cost computed above.
- Exclude episodes with residuals below the 1st percentile or above the 99th percentile of the residual distribution.
- Renormalize all remaining episodes by multiplying their cost by the ratio of the average observed episode cost and the average winsorized expected cost when
excluding outliers.
Calculate Measure Scores
The revised MSPB clinician measure is calculated for each clinician (TIN-NPI) or clinician group practice (TIN) by (i) calculating the ratio of standardized observed episode costs to final expected episode costs and (ii) multiplying the average cost ratio across episodes for each TIN or TIN-NPI by the national average standardized episode cost. This method of cost ratio calculation allows for comparison of differences in observed and expected costs at the level of each individual episode before comparison at the clinician or clinician group level.
Step 1: Calculate risk-adjusted episode cost ratio
For each non-outlier episode, the episode’s total standardized observed cost is divided by the
episode’s final expected cost.
Step 2: Calculate the revised MSPB clinician measure for each TIN or TIN-NPI
After calculating each episode’s risk-adjusted cost ratio, average this cost ratios across all episodes for each TIN or TIN-NPI. Multiplying this average cost ratio by the national average episode cost (all total standardized costs averaged over the universe of attributed, non-outlier episodes) gives the revised MSPB clinician measure for each TIN or TIN-NPI. Multiplication of the ratio by national average cost per episode is done to convert the ratio into a figure that is more meaningful from a cost perspective by having the clinician’s average cost measure score represented as a dollar amount rather than a ratio. Figure 2 below displays a formula representing how the measure score for any attributed clinician (or clinician group practice) “j” can be represented mathematically.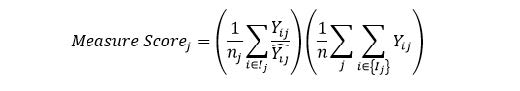
where:
| ??? | is the standardized payment for episode i and attributed clinician (or clinician group practice) j |
| ? ?? | is the expected standardized payment for episode i and clinician (or clinician group practice) j, as predicted from risk adjustment |
| ?? | is the number of episodes for clinician (or clinician group practice) j |
| ? | is the total number of TIN/TIN-NPI attributed episodes nationally |
| is all episodes i in the set of episodes attributed to clinician (or clinician group practice) j |
A higher measure score indicates that the observed episode costs are higher than expected for the care provided for the particular patients and episodes included in the calculation.
Appendix A. Summary of Refinements to the Revised MSPB Clinician Measure
This section summarizes differences between the current MSPB used in MIPS and the revised MSPB clinician measure. The revised measure differs from the current measure in three broad ways. First, the refined attribution methodology uses two different methods for episodes with medical and surgical MS-DRGs. Second, medical episodes are attributed first at the clinician group level and then at the clinician level, to recognize team-based nature of inpatient care. Third, service assignment involves the removal of certain services identified by expert stakeholder input to account for the more limited yet focused sphere of influence for clinicians as opposed to hospitals. Table A-1 below summarizes the refinements to the revised MSPB clinician measure.
| Refinement | Current MSPB measure | Revised MSPB clinician measure |
|---|---|---|
| Attribution | Attributed first at the clinician (TIN-NPI) level | Attributed medical episodes first at the clinician group (TIN) level and then at the clinician (TIN-NPI) level |
| Attributed each episode to the clinician billing the plurality of costs for Medicare Part B services rendered during an index admission | Separate attribution methods for medical and surgical episodes:
| |
| Service Assignment | All-cost measure that included all Medicare Parts A and B claims paid during the period from three days prior to the index admission through 30 days after discharge | Unrelated services specific to groups of DRGs aggregated by MDC level are excluded Examples include:
|
Appendix B. Illustrations of Attribution for Medical and Surgical MS-DRG Episodes
This appendix provides some further details and examples of attribution for episodes with medical and surgical MS-DRGs.
Medical MS-DRG Episode Attribution
An episode with a medical MS-DRG is attributed to a:
- TIN if that TIN billed at least 30 percent of the E&M claims billed during the inpatient stay, and to a
- TIN-NPI if a clinician within an attributed TIN billed at least one E&M claim that was used to determine the episode’s attribution to the TIN.
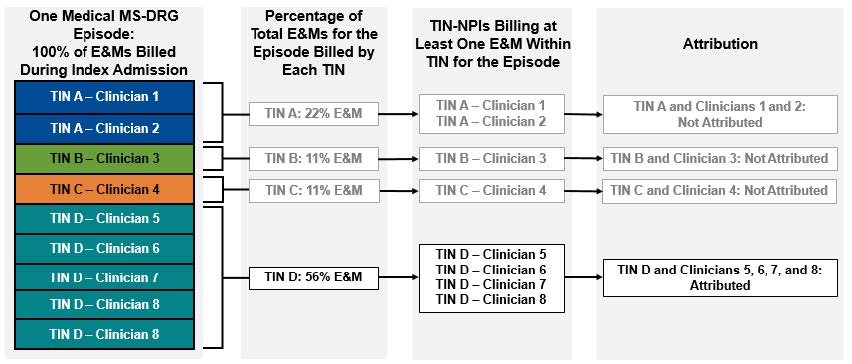
In the example shown above, the stacked, colored boxes on the left represent nine E&M claims billed by eight different clinicians (Clinicians 1 through 8) across four TINs (TINs A through D) during the index admission for one medical MS-DRG episode. Clinicians 1 through 7 billed one E&M claim, and Clinician 8 billed two E&M claims under TIN D. The next set of boxes to the right of the colored boxes shows the percentage of total E&Ms for that index admission billed by each of the four TINs. Moving right, the next set of boxes lists the clinicians within each of the four TINs who had billed at least one E&M during the index admission. Finally, the last set of boxes shows a summary of how this affects attribution.
Only TIN D billed at least 30 percent of the E&M codes during the index admission. This means:
- At the TIN level, only TIN D is attributed this episode.
- TINs A, B, and C did not meet the 30 percent threshold, so they are not attributed this episode.
- At the TIN-NPI level, each TIN-NPI (Clinicians 5, 6, 7, and 8) billing at least one E&M claim within TIN D is attributed this episode.
- TINs A, B, and C did not meet the 30 percent threshold, so the TIN-NPIs billing within them are not attributed this episode.
Surgical MS-DRG Episode Attribution
An episode with a surgical MS-DRG is attributed to a:
- TIN if that TIN billed the relevant CPT/HCPCS code determined as related to the surgical MS-DRG, and to a
- TIN-NPI if that clinician billed the relevant CPT/HCPCS code determined as related to the surgical MS-DRG.
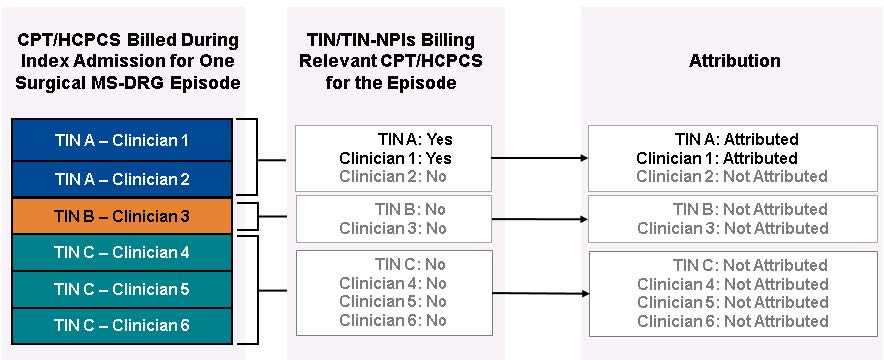
In the example shown above, the stacked, colored boxes on the left represent six CPT/HCPCS codes billed by six different clinicians (Clinicians 1 through 6) across three TINs (TINs A through C) during the index admission for one surgical MS-DRG episode. The next set of boxes to the right of the colored boxes shows whether each TIN/TIN-NPI billed a relevant or a non-relevant CPT/HCPCS code to the episode’s surgical MS-DRG. Finally, the last set of boxes shows a summary of how this affects attribution.
- Only TIN A billed the relevant CPT/HCPCS to the episode’s surgical MS-DRG during the index admission. This means that only TIN A is attributed this episode.
- TINs B and C did not bill any relevant CPT/HCPCS, so they are not attributed this episode.
- At the TIN-NPI level, only Clinician 1, who billed the relevant CPT/HCPCS code within TIN A, is attributed this episode.
- Clinicians 2 through 6 did not bill any relevant CPT/HCPCS codes, so they are not attributed this episode.