Introduction
This document details the methodology for the revised Total Per Capita Cost (TPCC) measure. The methodology should be reviewed along with the Measure Codes List file, which contains the medical codes used in constructing the measure.
Measure Description
The revised TPCC measures the overall cost of care delivered to a beneficiary with a focus on the primary care they receive from their provider(s). The measure is a payment-standardized, risk-adjusted, and specialty-adjusted measure. The revised measure is attributed to clinicians, who are identified by their unique Taxpayer Identification Number and National Provider Identifier pair (TIN-NPI) and clinician groups, identified by their TIN number. The revised TPCC measure can be attributed at the TIN or TIN-NPI level.
Measure Rationale
The TPCC measure is an important means of measuring Medicare spending, as health expenditures continue to increase in the United States. Total health care spending is estimated to have increased by 4.6 percent in 2017, reaching $3.5 trillion.2 Spending for Medicare, which is still predominantly paid on a fee-for-service (FFS) basis, grew by 3.6 percent, reaching $672.1 billion. Spending on services for physicians and other health professionals totaled $69.9 billion and accounted for 15 percent of Medicare FFS spending in 2016. The revised TPCC measure specifically focuses on the importance of successful payment models for primary care management. Effective primary care management can support Medicare savings in a number of ways, including through improvements in the treatment of chronic conditions by obviating the need for high-cost hospital or emergency department services. More effective primary care management can also direct a greater proportion of patients to lower hospital costs for the inpatient services. Given the potential for decreasing spending through improvements in primary care delivery, the TPCC measure allows for a savings opportunity by capturing the broader healthcare costs influenced by primary care.
A TPCC measure was originally used in the Physician Value-Based Payment Modifier (VM) Program and reported in the annual Quality and Resource Use Reports (QRURs). With the introduction of the Quality Payment Program, the current TPCC was finalized with minor adaptations from VM and added to MIPS. Subsequent Final Rules have noted that current TPCC and MSPB measures would be refined based on stakeholder input.
A technical expert panel (TEP) provided high-level guidance for the refinement of the measure at meetings in August 2017 and May 2018. The TEP consisted of 19 members from diverse backgrounds, including clinicians, healthcare providers, academia, and patient advocacy organizations. The revised TPCC measure underwent Field Testing in October-November 2018. A public comment period accompanied Field Testing, during which stakeholders reviewed and provided feedback on the TPCC Field Test Reports and the publicly posted supplementary documentation. Following Field Testing, the TEP reconvened in November 2018 to guide further measure refinement to address stakeholder feedback received through the public comment period.
Beneficiary Exclusion Criteria
Beneficiaries are excluded from the measure population if they meet any of the following conditions:
- They were not enrolled in both Medicare Part A and Part B for every month during the measurement period, unless part year enrollment was the result of new enrollment or death.
- They were enrolled in a private Medicare health plan (e.g., a Medicare Advantage or a Medicare private FFS plan) for any month during the measurement period.
- They resided outside the United States or its territories during any month of the measurement period.
- They are covered by the Railroad Retirement Board.
Measure Numerator:
The numerator for the measure is the sum of the risk-adjusted, payment-standardized, and specialty-adjusted Medicare Parts A and B costs across all beneficiary months attributed to a TIN or TIN-NPI during the measurement period.
Measure Denominator:
The denominator for the measure is the number of beneficiary months attributed to a TIN or TIN-NPI during the measurement period.
Data Sources
The revised TPCC measure uses the following data sources:
- Medicare Parts A and B claims data from the Common Working File (CWF),
- Enrollment Data Base (EDB),
- Common Medicare Environment (CME),
- Long Term Care Minimum Data Set (LTC MDS), and
- Provider Enrollment, Chain, and Ownership System (PECOS).
Quick Reference: Methodology Steps
There are two overarching processes in calculating revised MSPB clinician measure scores: episode construction (Steps 1-3) and measure calculation (Steps 4-6). This section provides a brief summary of these processes, and Section 4.0 describes them in detail.
- Identify candidate events. A candidate event identifies the start of a primary care relationship between a clinican and beneficiary. A candidate event is defined using select evaluation and management (E&M) CPT/HCPCS codes for outpatient physician visit, termed E&M primary care service, paired with one or more additional service(s) indicative of general primary care that together trigger the opening of a risk window.
- Apply service category and specialty exclusions. Clinicians are excluded from attribution if they meet the criteria for one or more service exclusions in the following categories: global surgery, anesthesia, therapeutic radiation, and chemotherapy. Clinicians are also excluded based on their HCFA Specialty designation, if they identify as one or more of the 56 specialties in the specialty exclusion list.
- Construct risk windows. The risk window begins on the date of the candidate event and continues until one year after that date. A beneficiary’s costs are attributable to a clinician during months where the risk window and measurement period overlap.
- Attribute months to TINs and TIN-NPIs. After service category and specialty exclusions are applied, all beneficiary costs occurring during the covered months are attributed to the remaining eligible TINs. For TIN-NPI attribution, only the TIN-NPI responsible for the majority share, or plurality, of candidate events provided to the beneficiary within the TIN is attributed that beneficiary’s costs for their respective candidate events.

- Calculate payment-standardized monthly observed costs. Monthly observed costs are payment standardized to account for differences in Medicare payments for the same service(s) across Medicare providers. All standardized cost from services starting in a beneficiary month are assigned.
- Calculate risk-adjusted monthly costs. Risk adjustment accounts for beneficiary-level risk factors that can affect medical costs, regardless of the care provided. After costs are risk- adjusted, winsorization is applied to reduce the effect of outliers.
- Apply specialty adjustment to risk-adjusted costs. A specialty adjustment is applied to monthly risk-adjusted costs to account for the fact that costs vary across specialties and across TINs with varying specialty compositions.
- Calculate the measure score. Calculate the average payment-standardized, risk-adjusted, and specialty-adjusted monthly costs across all beneficiary months in the measurement period attributed to a TIN or TIN-NPI for the measure score.
Quick Reference: Specifications
This page provides a quick, at-a-glance reference for the revised TPCC measure specifications. The full list of codes and logic used to define each component can be found within the Measure Codes List file.
| Candidate Event: Which patients are included in the measure? | |
| A candidate event is defined as a pair of services billed by the clinician to the beneficiary within a short period of time. A candidate event marks the start of a primary care relationship between a beneficiary and a clinician. | |
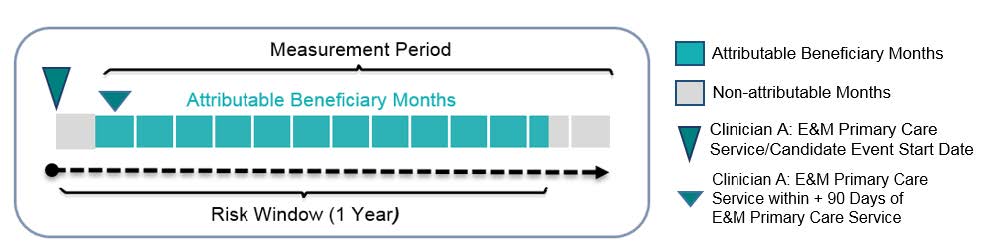
| Risk Window: When is a clinician responsible for the beneficiary costs? | |
| Risk window is a year-long period that begins on the date of the candidate event. | |
| Beneficiary Months Attribution: How is the revised TPCC measure attributed? | |
| The measurement period is a static calendar year that is divided into 13 four-week blocks called beneficiary months. Beneficiary months that occur during a risk window and the measurement period are counted towards a clinician’s (clinician group’s) measure scores. These beneficiary months are attributed to the TIN billing the initial E&M primary care service. For TIN-NPI-level attribution, only the TIN-NPI responsible for the plurality (largest share) of candidate events provided to the beneficiary within the TIN is attributed the beneficiary months. | |
| Service Assignment: Which services are included in the measure? | |
| Revised TPCC is an all-cost measure. | |
| Risk Adjustors: How does TPCC adjust for beneficiary-level risk factors that can affect medical costs? | Exclusions: Which populations are excluded from the measure? |
| Beneficiary risk score is calculated using CMS-ESRD V21 models (Dialysis New Enrollee Model, Dialysis Community Model) and CMS-HCC V22 models (New Enrollee Model, Community Model, Institutional Model) Risk adjustors included in the CMS-HCC risk adjustment models include the following:
|
|
Detailed Measure Calculation Methodology
This section describes the construction of the revised TPCC measure in more detail: Section 4.1 outlines the construction and attribution of beneficiary months to clinicians and Section 4.2 outlines measure calculation.
Measure Attribution
This section outlines in detail the following steps in measure attribution:
Step 1: Identify Candidate Events
Step 2: Apply Service Category and Specialty Exclusions
Step 3: Construct Risk Windows
Step 4: Attribute Beneficiary Months to TINs and TIN-NPIs
Step 1: Identify Candidate Events
A candidate event is used to indicate the start of a primary care relationship between a clinician and beneficiary and is identified by the occurrence of two Part B Physician/Supplier (Carrier) claims with particular CPT/HCPCS services billed in close proximity. There are two different sets of CPT/HCPCS codes used: E&M primary care services and primary care services.
E&M primary care services are a specific set of evaluation and management codes for physician visits in the outpatient setting, physician office, nursing facility, or assisted living.
Primary care services are a broader list of services related to routine primary care and generally fall into the following categories:
- Durable Medical Equipment (DME) and Supplies
- Electrocardiogram
- Laboratory – Chemistry and Hematology
- Other Diagnostic Procedures (Interview, Evaluation, Consultation)
- Other Diagnostic Radiology and Related Techniques
- Prophylactic Vaccinations and Inoculations
- Routine Chest X-ray
- Clinical Labs
- Preventive Services
To identify a candidate event, firstly, an initial E&M primary care service billed on Part B Physician/Supplier (Carrier) claim is identified. This E&M primary care service is not considered if it occurs during a beneficiary’s stay at a Critical Access Hospital (CAH), Inpatient Facility, or Skilled Nursing Facility (SNF). Secondly, in addition to the initial E&M primary care service, at least one of the following services should be billed to confirm the candidate event:
- From any TIN within +/- 3 days: Another primary care service,
- From the same TIN within + 90 days: A second E&M primary care service OR another primary care service
See the “Prim_Care_E&Ms” and the “Prim_Care_Services” tabs of the revised TPCC Measure Codes List file for the list of the Current Procedural Terminology/Healthcare Common Procedure Coding System (CPT/HCPCS) codes that identify E&M primary care services and primary care services, respectively.
Step 2: Apply Service Category and Specialty Exclusions
Once candidate events are identified, TIN-NPIs can be attributed based on their involvement in the candidate event. The TIN-NPI responsible for a candidate event is found on the initial E&M primary care service claim of the candidate event. Some TIN-NPIs are excluded from attribution if they meet one of two types of exclusions: service category exclusions and specialty exclusions. Candidate events belonging to TIN-NPIs who meet any of these exclusions are removed from attribution and measure calculation for both the TIN-NPI and their respective TIN.
Step 2.1: Exclude Clinicians Based on Service Category Exclusions
A TIN-NPI and their candidate events are removed from attribution if a clinician met any of the following four service category thresholds for the same beneficiary:
- At least 15 percent of the clinician’s candidate events are comprised of 10-day or 90-day global surgery services.
- At least 5 percent of the clinician’s candidate events are comprised of anesthesia services.
- At least 5 percent of the clinician’s candidate events are comprised of therapeutic radiation services.
- At least 10 percent of the clinician’s candidate events are comprised of chemotherapy services.
The list of CPT/HCPCS codes used for each of the service exclusions can be found in the tabs of the TPCC Measure Codes List file labelled: “HCPCS_Surgery,” “HCPCS_Anesthesia,” “HCPCS_Ther_Rad,” and “HCPCS_Chemo.”
Step 2.2: Exclude Clinicians Based on Specialty Exclusions
After service category exclusions are applied, clinicians who would not reasonably be responsible for providing primary care are excluded from attribution of the revised TPCC measure. This exclusion aims to keep primary care specialists and internal medicine sub-specialists who frequently manage patients with chronic conditions falling in their areas of specialty. The excluded specialties list contains 56 specialties that fall into the following broad categories:
- Surgical sub-specialties
- Non-physicians without chronic management of significant medical conditions
- Internal medicine sub-specialties with additional highly procedural sub-specialization
- Internal medicine specialties that practice primarily inpatient care without chronic care management
- Pediatricians who do not typically practice adult medicine
The list of HCFA Specialty codes that identify clinicians that are included or excluded from the measure attribution can be found in the “Eligible_Clinicians” tab of the TPCC Measure Codes List.
As with service category exclusions described in Step 2.1, candidate events for clinicians in excluded specialties are removed from attribution and measure calculation for both the TIN-NPI and their respective TIN.
Step 3: Construct Risk Windows
Candidate events that are not excluded initiate the opening of a risk window, a year-long period that begins on the date of the initial E&M primary care service of the candidate event. The measurement period is divided into 13 four-week blocks called beneficiary months. Beneficiary months during the risk window are considered attributable if they occur during the measurement period. In the event that a risk window begins or ends with a partially covered month, only the portion during the risk window and the measurement period is considered for attribution. Appendix C contains examples of overlapping risk windows initiated by one or multiple TINs for the same beneficiary and explains how this overlap is addressed.
Step 4: Attribute Beneficiary Months to TINs and TIN-NPIs
Beneficiary months for a single beneficiary are attributed to a TIN or TIN-NPI according to the following steps:
- For attribution at the TIN level:
- Identify the TIN billing the initial E&M primary care service claim of each candidate event.
- Determine beneficiary months that fall within the risk windows of the candidate events that were initiated by the TIN and overlap the measurement period and attribute those beneficiary months to the TIN.
- For attribution at the TIN-NPI level:
- Identify the TIN-NPI billing the initial E&M primary care service claim of each candidate events.
- Determine beneficiary months that fall within the risk windows of the candidate events that were initiated by the TIN-NPI and that overlap the measurement period.
- Identify the TIN-NPI within an attributed TIN that is responsible for the plurality of candidate events provided to the beneficiary. If two or more TIN-NPIs under a TIN provide the same proportion of candidate events to a beneficiary, attribute the beneficiary to the TIN-NPI that provided the earliest candidate event.
- Attribute only the beneficiary months from candidate events that the TIN-NPI is responsible for initiating, which is not necessarily all candidate events attributed to the TIN for that beneficiary.
All attributed beneficiary months for all beneficiaries are used for the measure calculation for each TIN and TIN-NPI.
Step 4.2: Measure Calculation
This section outlines the following steps in measure calculation:
Step 5: Calculate Payment-Standardized Monthly Observed Costs
Step 6: Risk-Adjust Monthly Costs
Step 7: Specialty Adjust Monthly Costs
Step 8: Calculate the revised TPCC Measure
Step 5: Calculate Payment-Standardized Monthly Observed Costs
Monthly observed cost for attributed beneficiary months is the sum of all service costs billed for a particular beneficiary during a beneficiary month. Monthly observed costs are standardized to account for differences in Medicare payments for the same service(s) across Medicare providers. Payment standardization accounts for differences in Medicare payment unrelated to the care provided, such as those from payment adjustments supporting larger Medicare program goals (e.g. indirect medical education add-on payments) or variation in regional healthcare expenses as measured by hospital wage indexes and geographic price cost indexes (GPCIs). Standardized costs that occur during partially covered months are pro-rated, based on the portion of the month covered by the risk window.
Step 6: Risk-Adjust Monthly Costs
Risk adjustment accounts for beneficiary-level risk factors that can affect medical costs, regardless of the care provided. To ensure that the model measures the influence of health status (as measured by diagnoses) on the treatment provided (costs incurred) rather than capturing the influence of treatment on a beneficiary’s health status, the risk adjustment model uses risk factors from the year prior to a beneficiary month. Separate CMS-HCC models exist for new enrollees, continuing enrollees, enrollees in long-term institutional settings, and enrollees with End-Stage Renal Disease (ESRD).
Risk Adjustment Models
The CMS Hierarchical Condition Category Version 22 (CMS-HCC V22) 2016 Risk Adjustment models are used for beneficiaries without ESRD. Specifically,
- The new enrollee model is used for beneficiaries that have fewer than 12 months of Medicare medical history. The model accounts for each beneficiary’s age, sex, disability status, original reason for Medicare entitlement (age or disability), and Medicaid eligibility.
- The community model is used for beneficiaries that have least 12 months of Medicare medical history. The model includes the same demographic information as the new enrollee model but also accounts for clinical conditions as measured by HCCs.
- The institutional model is used for beneficiaries who were in long-term institutional settings. The model includes demographic variables, clinical conditions as measured by HCCs, and various interaction terms.
The CMS-ESRD Version 21 (CMS-ESRD V21) 2016 Risk Adjustment models are used for ESRD beneficiaries receiving dialysis. Specifically,
- The dialysis new enrollee model is used for ESRD beneficiaries that have fewer than 12 months of Medicare medical history. The model accounts for each beneficiary’s age, sex, disability status, original reason for Medicare entitlement (age or disability), Medicaid eligibility, and ESRD.
- The dialysis community model is used for ESRD beneficiaries that have at least 12 months of Medicare medical history. The model includes the same demographic information as the new enrollee model but also accounts for clinical conditions as measured by HCCs.
The “HCC_Risk_Adjust” tab of the Measure Codes List file lists all variables included in the CMS-ESRD V21 and the CMS-HCC V22 risk adjustment models.
Risk Score Calculation
The CMS-ESRD V21 and CMS-HCC V22 models generate a risk score for each beneficiary that summarizes the beneficiary’s expected cost of care relative to other beneficiaries. Risk scores for ESRD beneficiaries are normalized to be on a comparable scale with the HCC V22 risk scores.
- A risk score equal to 1 indicates risk associated with expenditures for the average beneficiary nationwide.
- A risk score greater than 1 indicates above average risk.
- A risk score less than 1 indicates below average risk.
The risk-adjusted total for each covered month at the TIN or TIN-NPI level is calculated according to the following steps:
- Calculate CMS risk score for each beneficiary month using diagnostic data from the year prior to the month. This risk score is normalized by dividing by the average risk score for all beneficiary months.
- Divide observed costs for each beneficiary month by the normalized risk score to obtain risk-adjusted monthly costs.
- Winsorize risk-adjusted monthly costs at the 99th percentile by assigning the 99th percentile of monthly costs to all attributable beneficiary months with costs above the 99th percentile.
- Normalize monthly costs to account for differences in expected costs based on the number of clinician groups to which a beneficiary is attributed in a given month.
Step 7: Specialty Adjust Monthly Costs
The specialty adjustment for the revised TPCC measure is a cost adjustment applied to account for the fact that costs vary across specialties and across TINs with varying specialty compositions. An example of the specialty adjustment calculation is available in Appendix E. The specialty adjustment at the TIN and TIN-NPI levels is calculated as follows:
- Calculate the average risk-adjusted monthly cost for each TIN and TIN-NPI by averaging risk-adjusted monthly cost across all attributed beneficiary months.
- Calculate the national specialty-specific expected cost for each specialty as the weighted average of TIN/TIN-NPI’s risk-adjusted monthly cost.
- Define the weight for each TIN/TIN-NPI as the percentage of clinicians with that specialty multiplied by the total number of beneficiary months attributed to the TIN/TIN-NPI multiplied by the number of clinicians with that specialty.
- There will only be one specialty designation for a TIN-NPI. Therefore, the percentage of clinicians with a specialty and number of clinicians with a specialty will always be equal to 1.
- Calculate the specialty-adjustment factor for each TIN or TIN-NPI as follows:
- Multiply the national specialty-specific expected cost for each specialty by the respective specialty’s share of Part B payment within a TIN or TIN-NPI.
- Sum the weighted share of national specialty-specific expected cost calculated in the previous step across all the specialties under a given TIN or TIN-NPI.
Step 8: Calculate the Revised TPCC Measure Score
Calculate final risk-adjusted, specialty-adjusted cost measure by dividing each TIN and TIN-NPI’s average risk-adjusted monthly cost by their specialty-adjustment factor and multiply this ratio by the average non-risk-adjusted, winsorized observed cost across the total population of attributed beneficiary months.
The clinician-level or clinician group practice-level measure score for any attributed clinician (or clinician group practice) “j” can be represented mathematically as: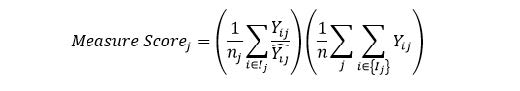
where:
| ??? | is the standardized payment for episode i and attributed clinician (or clinician group practice) j |
| ? ?? | is the expected standardized payment for episode i and clinician (or clinician group practice) j, as predicted from risk adjustment |
| ?? | is the number of episodes for clinician (or clinician group practice) j |
| ? | is the total number of TIN/TIN-NPI attributed episodes nationally |
| is all episodes i in the set of episodes attributed to clinician (or clinician group practice) j |
A higher measure score indicates that the observed beneficiary month costs are higher than the expected costs for the care provided by the given specialist for the particular patients and beneficiary months included in the calculation.
Appendix A. Refinements to the Current TPCC Measure
This appendix summarizes differences between the current TPCC measure used in the 2017 MIPS performance period and the revised TPCC measure. The revised measure differs from the MIPS version of the measure in three broad ways. First, the attribution method allows for the attribution of beneficiaries to multiple clinicians and clinician groups. Second, the revised measure only assigns cost after the start of the clinician-patient relationship. Third, the new risk adjustment methodology determines beneficiary’s risk score for each covered month measured using risk factors from the year prior to the covered month.
| Refinement | Current TPCC measure in use for MIPS | Revised TPCC measure |
|---|---|---|
| Attribution | Under the current methodology, beneficiaries are attributed as follows:
| New attribution method better identifies the existence of a primary care relationship between multiple clinician groups and beneficiaries. Specifically, the attribution method has been refined as follows:
|
| Cost Assignment | The entire annual cost during the measurement period for a beneficiary is assigned to the attributed clinician regardless of when the patient-beneficiary relationship started, in some cases leading to assignment of cost to a clinician prior to ever seeing the beneficiary. | Each attributable event initiates a one-year risk window during which a beneficiary’s costs may be attributable to a clinician. Therefore, cost is only assigned after the clinician has seen the beneficiary. |
| Risk adjustment “lookback” period | Determine beneficiary’s risk score using risk factors from the year prior to measurement period. | Determine beneficiary’s risk score using risk factors for each covered month measured usi |