MIPS Clinical Quality Measures (CQMS)
MEASURE TYPE: Patient-Reported Outcome-Based Performance Measure – High Priority
Description
For patients 18 years of age or older who had a lumbar discectomy/laminectomy or fusion procedure, leg pain is rated by the patient as less than or equal to 3.0 OR an improvement of 5.0 points or greater on the Visual Analog Scale (VAS) Pain scale or a numeric pain scale at three months (6 to 20 weeks) for discectomy/laminectomy or at one year (9 to 15 months) postoperatively for lumbar fusion patients. Rates are stratified by procedure type; lumbar discectomy/laminectomy or fusion procedure.
Instructions:
This measure is to be submitted each time a patient undergoes a lumbar discectomy/laminectomy or fusion during the denominator identification period. This measure may be submitted by Merit-based Incentive Payment System (MIPS) eligible clinicians who perform the quality actions described in the measure based on the services provided and the measure-specific denominator coding.
NOTE: This measure is a target-based measure with two ways to meet the numerator; either a postoperative VAS Pain or Numeric pain score that is less than or equal to 3.0 OR an improvement of 5.0 points or greater from the preoperative to postoperative score. It is expressed as a proportion or rate. Patients having received a lumbar discectomy/laminectomy or fusion procedure who are not assessed for leg pain postoperatively remain in the denominator and are considered as not meeting the target. The measure intent is that MIPS eligible clinicians will submit all denominator eligible procedures for performance calculation.
This measure will be calculated with 2 performance rates:
- Percentage of lumbar discectomy/laminectomy procedures for which the patient reports leg pain less than or equal to 3.0 OR an improvement of 5.0 points or greater on the VAS or Numeric Pain scale at three months (6 to 20 weeks) postoperatively
- Percentage of lumbar fusion procedures for which the patient reports leg painless than or equal to 3.0 OR an improvement of 5.0 points or greater on the VAS or Numeric Pain scale at one year (9 to 15 months) postoperatively after lumbar fusion.
A weighted average, which is the sum of the performance numerator values divided by the sum of performance denominator values, will be used to calculate performance.
Measure Submission Type
Measure data may be submitted by individual MIPS eligible clinicians, groups, or third-party intermediaries. The listed denominator criteria are used to identify the intended patient population. The numerator options included in this specification are used to submit the quality actions as allowed by the measure. The quality data codes listed do not need to be submitted by MIPS eligible clinicians, groups, or third-party intermediaries that utilize this modality for submissions; however, these codes may be submitted for those third-party intermediaries that utilize Medicare Part B claims data. For more information regarding Application Programming Interface (API), please refer to the Quality Payment Program (QPP) website.
Denominator (Submission Criteria 1):
Patients with lumbar discectomy/laminectomy procedure. Patients 18 years of age or older as of January 1 of the denominator identification period who had a lumbar discectomy/laminectomy procedure performed during the denominator identification period
Definition:
Denominator Identification Period – The twelve-month period in which eligible patients have a procedure. This allows for enough time for a follow-up assessment to occur during the performance period. The “denominator identification period” includes dates of procedure of 1/1/2023 to 12/31/2023.
Denominator Criteria (Eligible Cases):
Patients aged ≥ 18 years by January 1 of the Denominator Identification Period
AND
Patient procedure during the denominator identification period (CPT): 63005, 63012, 63017, 63030, 63042, 63047
WITHOUT
Telehealth Modifier (including but not limited to): GQ, GT, 95, POS 02, POS 10
AND NOT
Denominator Exclusions:
Patient had a lumbar fusion on the same date as the discectomy/laminectomy procedure (CPT): 22533, 22558, 22586, 22612, 22630, 22633
AND NOT
Patient had cancer, acute fracture or infection related to the lumbar spine OR patient had neuromuscular, idiopathic, or congenital lumbar scoliosis: M1051
Patients with a diagnosis of lumbar spine region cancer at the time of the procedure – The following codes would be sufficient to define the Denominator Exclusion (M1051) of lumbar spine region cancer: C41.2, C41.4, C79.51, C79.52, D16.6, D16.8, D48.0, D49.2
Patients with a diagnosis of acute lumbar spine region fracture at the time of the procedure – The following codes would be sufficient to define the Denominator Exclusion (M1051) of lumbar spine region fracture: M48.44XA, M48.45XA, M48.46XA, M48.47XA, M48.48XA, M48.54XA, M48.55XA, M48.56XA, M48.57XA, M48.58XA, S22.060A, S22.060B, S22.061A, S22.061B, S22.062A, S22.062B, S22.068A, S22.068B, S22.069A, S22.069B, S22.070A, S22.070B, S22.071A, S22.071B, S22.072A, S22.072B, S22.078A, S22.078B, S22.079A, S22.079B, S22.080A, S22.080B, S22.081A, S22.081B, S22.082A, S22.082B, S22.088A, S22.088B, S22.089A, S22.089B, S24.103A, S24.104A, S24.113A, S24.114A, S24.133A, S24.134A, S24.143A, S24.144A, S24.153A, S24.154A, S32.000A, S32.000B, S32.001A, S32.001B, S32.002A, S32.002B, S32.008A, S32.008B, S32.009A, S32.009B, S32.010A, S32.010B, S32.011A, S32.011B, S32.012A, S32.012B, S32.018A, S32.018B, S32.019A, S32.019B, S32.020A, S32.020B, S32.021A, S32.021B, S32.022A, S32.022B, S32.028A, S32.028B, S32.029A, S32.029B, S32.030A, S32.030B, S32.031A, S32.031B, S32.032A, S32.032B, S32.038A, S32.038B, S32.039A, S32.039B, S32.040A, S32.040B, S32.041A, S32.041B, S32.042A, S32.042B, S32.048A, S32.048B, S32.049A, S32.049B, S32.050A, S32.050B, S32.051A, S32.051B, S32.052A, S32.052B, S32.058A, S32.058B, S32.059A, S32.059B, S32.10XA, S32.10XB, S32.110A, S32.110B, S32.111A, S32.111B, S32.112A, S32.112B, S32.119A, S32.119B, S32.120A, S32.120B, S32.121A, S32.121B, S32.122A, S32.122B, S32.129A, S32.129B, S32.130A, S32.130B, S32.131A, S32.131B, S32.132A, S32.132B, S32.139A, S32.139B, S32.14XA, S32.14XB, S32.15XA, S32.15XB, S32.16XA, S32.16XB, S32.17XA, S32.17XB, S32.19XA, S32.19XB, S32.2XXA, S32.2XXB, S32.9XXA, S32.9XXB, S34.101A, S34.102A, S34.103A, S34.104A, S34.105A, S34.109A, S34.111A, S34.112A, S34.113A, S34.114A, S34.115A, S34.119A, S34.121A, S34.122A, S34.123A, S34.124A, S34.125A, S34.129A, S34.131A, S34.132A, S34.139A, S34.3XXA
Patients with a diagnosis of lumbar spine region infection at the time of the procedure – The following codes would be sufficient to define the Denominator Exclusion (M1051) of lumbar spine region infection: M46.25, M46.26, M46.27, M46.28, M46.35, M46.36, M46.37, M46.38, M46.45, M46.46, M46.47, M46.48, M46.55, M46.56, M46.57, M46.58
Patients with a diagnosis of lumbar neuromuscular, idiopathic, or congenital scoliosis – The following codes would be sufficient to define the Denominator Exclusion (M1051) of neuromuscular, idiopathic, or congenital scoliosis: M41.05, M41.06, M41.07, M41.08, M41.45, M41.46, M41.47, M41.115, M41.116, M41.117, M41.125, M41.126, M41.127, M41.25, M41.26, M41.27, Q67.5, Q76.3
Numerator (Submissions Criteria 1):
All eligible patients whose leg pain is less than or equal to 3.0 OR an improvement of 5.0 points or greater on the VAS or Numeric Pain scale at three months (6 to 20 weeks) postoperatively
Definitions:
Measure Assessment Period (Performance Period) – The period of time following the procedure date in which a postoperative VAS pain scale score is obtained.
Preoperative Assessment VAS or Numeric Pain – A preoperative VAS or Numeric pain scale score can be obtained from the patient any time up to three months pre-operatively, inclusive of the date of the procedure. Assessment scores obtained more than three months before the procedure will not be used for measure calculation. If more than one preoperative VAS or Numeric was obtained, use the VAS or Numeric score that is the most recent and prior to the procedure.
Postoperative Assessment VAS or Numeric Pain – A postoperative VAS or Numeric pain scale score can be obtained from the patient three months (6 to 20 weeks) after the date of the procedure. Assessment scores obtained prior to 6 weeks and after 20 weeks postoperatively will not be used for measure calculation. If more than one postoperative VAS or Numeric score was obtained during the six to 20 weeks following the procedure, use the most recent score obtained during the allowable timeframe.
Visual Analog Scale – A “visual analog scale” is a continuous line indicating the continuum between two states of being.
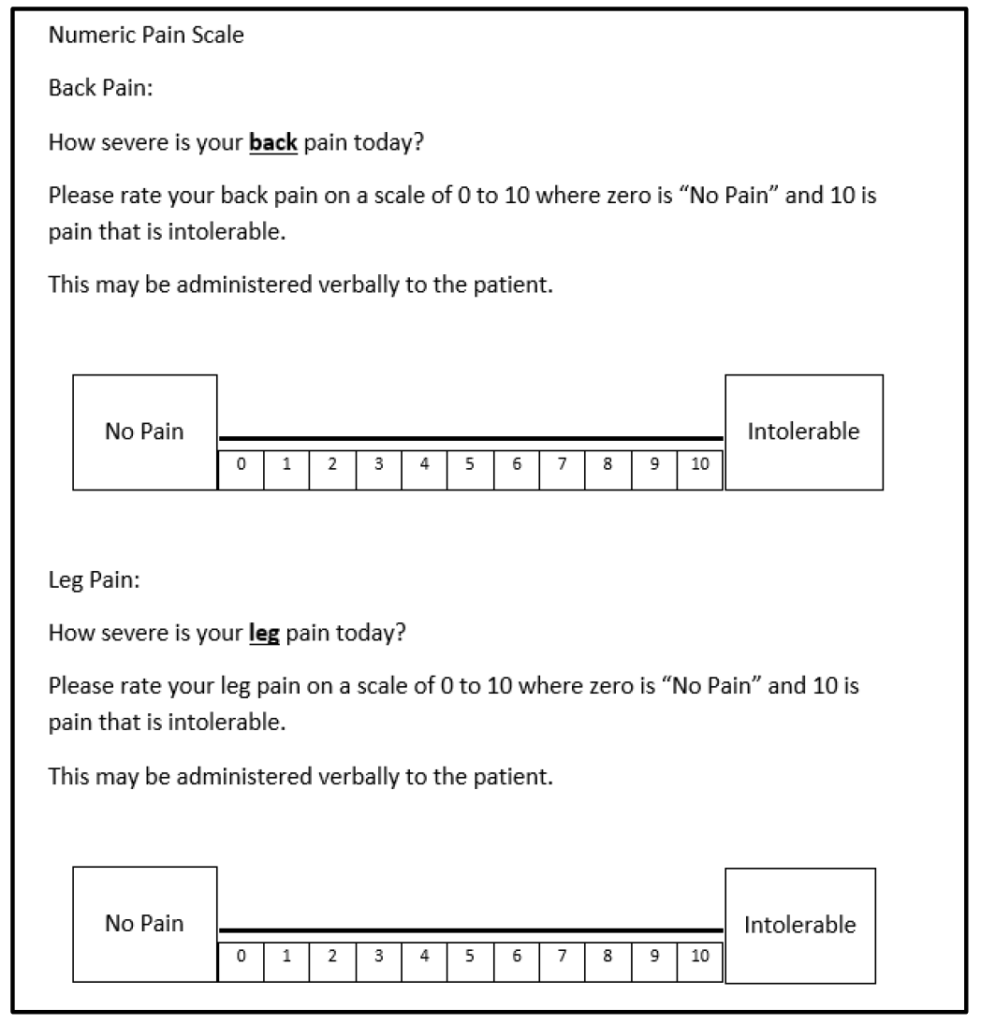
Numeric Pain Scale – a “numeric pain scale” is one that asks the patient to rate their pain on a scale of 0 to 10 where zero is “No Pain” and 10 is pain that is intolerable. This type of pain score tool can be administered verbally to the patient and because it does not involve a visual line, multiple modes of administration (e.g., phone, virtual visit, patient portal, verbally in-person, etc.) are acceptable.
Copies of the pain scale tools can be obtained at the following link: https://helpdesk.mncm.org/helpdesk/KB/View/17776810-spine-surgery-pro-tools
Leg Pain Target #1 – A patient who is assessed postoperatively at three months (6 to 20 weeks) after the procedure who rates their leg pain as less than or equal to 3.0.
Leg Pain Target #2 – A patient who does not meet Leg Pain Target #1 is assessed both preoperatively within 3 months prior to the procedure AND postoperatively at three months (6 to 20 weeks) after the procedure AND the improvement in leg pain is greater than or equal to 5.0 points.
NUMERATOR NOTE: It is recommended that both a preoperative and postoperative assessment tool be administered to the patient increasing the chances that one of the numerator targets will be met.
The following situations are those in which the numerator target cannot be reached and Performance Not Met G9949 or G2141 is submitted:
- VAS or Numeric Pain Scale is not administered postoperatively at three months (6 to 20 weeks)
- Leg pain is measured using a different patient reported tool
- Postoperative VAS or Numeric Pain Scale is administered less than six weeks or more than 20 weeks (3 month window)
- Postoperative VAS or Numeric value is greater than 3.0 and no valid preop to measure improvement
- Postoperative VAS or Numeric value is greater than 3.0 and preoperative VAS Pain Scale (to measure improvement) is administered beyond the three month timeframe prior to and including the date of procedure (e.g. 6 months before procedure)
Numerator Options:
Performance Met: Leg pain measured by the Visual Analog Scale (VAS) or Numeric pain scale at three months (6 – 20 weeks) postoperatively was less than or equal to 3.0 OR Leg pain measured by the Visual Analog Scale (VAS) or Numeric pain scale within three months preoperatively AND at three months (6 – 20 weeks) postoperatively demonstrated an improvement of 5.0 points or greater (G2140)
OR
Performance Not Met: Leg pain was not measured by the Visual Analog Scale (VAS) or Numeric pain scale at three months (6 – 20 weeks) postoperatively (G9949)
OR
Performance Not Met: Leg pain measured by the Visual Analog Scale (VAS) or Numeric pain scale at three months (6 – 20 weeks) postoperatively was greater than 3.0 AND Leg pain measured by the Visual Analog Scale (VAS) or Numeric pain scale within three months preoperatively AND at three months (6 – 20 weeks) postoperatively demonstrated improvement of less than 5.0 points (G2141)
Denominator (Submission Criteria 2):
Patients with lumbar fusion procedure. Patients 18 years of age or older as of October 1 of the denominator identification period who had a lumbar fusion procedure performed during the denominator identification period
Definition:
Denominator Identification Period – The twelve month period in which eligible patients have a procedure. This allows for enough time for a follow-up assessment to occur during the performance period. The “denominator identification period” includes dates of procedure 10/1/2022 to 9/30/2023.
Denominator Criteria (Eligible Cases):
Patients aged ≥ 18 years by October 1 of the Denominator Identification Period
AND
Patient procedure during the denominator identification period (CPT): 22533, 22558, 22586, 22612, 22630, 22633
WITHOUT
Telehealth Modifier (including but not limited to): GQ, GT, 95, POS 02, POS 10
Denominator Exclusions:
Patient had cancer, acute fracture or infection related to the lumbar spine OR patient had neuromuscular, idiopathic, or congenital lumbar scoliosis: M1051
Patients with a diagnosis of lumbar spine region cancer at the time of the procedure – The following codes would be sufficient to define the Denominator Exclusion (M1051) of lumbar spine region cancer- C41.2, C41.4, C79.51, C79.52, D16.6, D16.8, D48.0, D49.2
Patients with a diagnosis of acute lumbar spine region fracture at the time of the procedure – The following codes would be sufficient to define the Denominator Exclusion (M1051) of lumbar spine region fracture- M48.44XA, M48.45XA, M48.46XA, M48.47XA, M48.48XA, M48.54XA, M48.55XA, M48.56XA, M48.57XA, M48.58XA, S22.060A, S22.060B, S22.061A, S22.061B, S22.062A, S22.062B, S22.068A, S22.068B, S22.069A, S22.069B, S22.070A, S22.070B, S22.071A, S22.071B, S22.072A, S22.072B, S22.078A, S22.078B, S22.079A, S22.079B, S22.080A, S22.080B, S22.081A, S22.081B, S22.082A, S22.082B, S22.088A, S22.088B, S22.089A, S22.089B, S24.103A, S24.104A, S24.113A, S24.114A, S24.133A, S24.134A, S24.143A, S24.144A, S24.153A, S24.154A, S32.000A, S32.000B, S32.001A, S32.001B, S32.002A, S32.002B, S32.008A, S32.008B, S32.009A, S32.009B, S32.010A, S32.010B, S32.011A, S32.011B, S32.012A, S32.012B, S32.018A, S32.018B, S32.019A, S32.019B, S32.020A, S32.020B, S32.021A, S32.021B, S32.022A, S32.022B, S32.028A, S32.028B, S32.029A, S32.029B, S32.030A, S32.030B, S32.031A, S32.031B, S32.032A, S32.032B, S32.038A, S32.038B, S32.039A, S32.039B, S32.040A, S32.040B, S32.041A, S32.041B, S32.042A, S32.042B, S32.048A, S32.048B, S32.049A, S32.049B, S32.050A, S32.050B, S32.051A, S32.051B, S32.052A, S32.052B, S32.058A, S32.058B, S32.059A, S32.059B, S32.10XA, S32.10XB, S32.110A, S32.110B, S32.111A, S32.111B, S32.112A, S32.112B, S32.119A, S32.119B, S32.120A, S32.120B, S32.121A, S32.121B, S32.122A, S32.122B, S32.129A, S32.129B, S32.130A, S32.130B, S32.131A, S32.131B, S32.132A, S32.132B, S32.139A, S32.139B, S32.14XA, S32.14XB, S32.15XA, S32.15XB, S32.16XA, S32.16XB, S32.17XA, S32.17XB, S32.19XA, S32.19XB, S32.2XXA, S32.2XXB, S32.9XXA, S32.9XXB, S34.101A, S34.102A, S34.103A, S34.104A, S34.105A, S34.109A, S34.111A, S34.112A, S34.113A, S34.114A, S34.115A, S34.119A, S34.121A, S34.122A, S34.123A, S34.124A, S34.125A, S34.129A, S34.131A, S34.132A, S34.139A, S34.3XXA
Patients with a diagnosis of lumbar spine region infection at the time of the procedure – The following codes would be sufficient to define the Denominator Exclusion (M1051) of lumbar spine region infection- M46.25, M46.26, M46.27, M46.28, M46.35, M46.36, M46.37, M46.38, M46.45, M46.46, M46.47, M46.48, M46.55, M46.56, M46.57, M46.58
Patients with a diagnosis of lumbar neuromuscular, idiopathic, or congenital scoliosis – The following codes would be sufficient to define the Denominator Exclusion (M1051) of neuromuscular, idiopathic, or congenital scoliosis- M41.05, M41.06, M41.07, M41.08, M41.45, M41.46, M41.47, M41.115, M41.116, M41.117, M41.125, M41.126, M41.127, M41.25, M41.26, M41.27, Q67.5, Q76.3
Numerator (Submissions Criteria 2):
All eligible patients whose leg pain is less than or equal to 3.0 OR an improvement of 5.0 points or greater on the Visual Analog Scale (VAS) or Numeric Pain scale at one year (9 to 15 months) postoperatively
Definitions:
Measure Assessment Period (Performance Period) – The period of time following the procedure date that is in which a postoperative VAS or Numeric pain scale score is obtained.
Preoperative Assessment VAS or Numeric Pain – A preoperative VAS or Numeric pain scale score can be obtained from the patient any time up to three months preoperatively, inclusive of the date of the procedure. Assessment scores obtained more than three months before the procedure will not be used for measure calculation. If more than one preoperative VAS or Numeric score was obtained, use the VAS or Numeric score that is the most recent and prior to the procedure.
Postoperative Assessment or Numeric VAS Pain – A postoperative VAS or Numeric pain scale score can be obtained from the patient one year (9 to 15 months) after the date of procedure.
Assessment scores obtained prior to 9 months and after 15 months postoperatively will not be used for measure calculation. If more than one postoperative VAS or Numeric score was obtained during the 9 to 15 months following the procedure, use the most recent score obtained during the allowable timeframe.
Visual Analog Scale (VAS) – A “visual analog scale” is a continuous line indicating the continuum between two states of being.
Numeric Pain Scale – a “numeric pain scale” is one that asks the patient to rate their pain on a scale of 0 to 10 where zero is “No Pain” and 10 is pain that is intolerable. This type of pain score tool can be administered verbally to the patient and because it does not involve a visual line, multiple modes of administration (e.g., phone, virtual visit, patient portal, verbally in-person, etc.) are acceptable.
Copies of the pain scale tools can be obtained at the following link: https://helpdesk.mncm.org/helpdesk/KB/View/17776810-spine-surgery-pro-tools
Leg Pain Target #1 – A patient who is assessed postoperatively at one year (9 to 15 months) after the procedure rates their leg pain as less than or equal to 3.0.
Leg Pain Target #2 – A patient who does not meet Leg Pain Target #1 is assessed both preoperatively within 3 months prior to the procedure AND postoperatively one year (9 to 15 months) after the procedure AND the improvement in leg pain is greater than or equal to 5.0 points.
NUMERATOR NOTE: It is recommended that both a preoperative and postoperative assessment tool be administered to the patient increasing chances that one of the numerator targets will be met. The following situations are those in which the numerator target cannot be reached and Performance Not Met M1052 or G2147 is submitted:
- VAS Pain or Numeric Scale is not administered postoperatively at one year (9 to 15 months)
- Leg pain is measured using a different patient reported functional pain tool
- Postoperative VAS or Numeric Pain scale is administered less than 9 months or greater than 15 months (1 year window)
- Postoperative VAS or Numeric value is greater than 3.0 and no valid preoperative VAS Pain scale to measure improvement
- Postoperative VAS or Numeric value is greater than 3.0 and preoperative VAS or Numeric Pain scale (to measure improvement) is administered beyond the three month timeframe prior to and including the date of procedure (e.g. 6 months before procedure)
Numerator Options:
Performance Met: Leg pain as measured by the Visual Analog Scale (VAS) or Numeric pain scale at one year (9 to 15 months) postoperatively was less than or equal to 3.0 OR Leg pain measured by the Visual Analog Scale (VAS) or Numeric pain scale within three months preoperatively AND at one year (9 to 15 months) postoperatively demonstrated an improvement of 5.0 points or greater (G2146)
OR
Performance Not Met: Leg pain was not measured by the Visual Analog Scale (VAS) or Numeric pain scale at one year (9 to 15 months) postoperatively (M1052)
OR
Performance Not Met: Leg pain measured by the Visual Analog Scale (VAS) or Numeric pain scale at one year (9 to 15 months) postoperatively was greater than 3.0 AND Leg pain measured by the Visual Analog Scale (VAS) or Numeric pain scale within three months preoperatively AND at one year (9 to 15 months) postoperatively demonstrated improvement of less than 5.0 points (G2147)
RATIONALE:
Mechanical low back pain (LBP) remains the second most common symptom-related reason for seeing a physician in the United States. Of the US population, 85% will experience an episode of mechanical LBP at some point during their lifetime. Fortunately, the LBP resolves for the vast majority within 2-4 weeks.
For individuals younger than 45 years, mechanical LBP represents the most common cause of disability and is generally associated with a work-related injury. For individuals older than 45 years, mechanical LBP is the third most common cause of disability, and a careful history and physical examination are vital to evaluation, treatment, and management (Hills et al 2022).
Overall, spine surgery rates have declined slightly from 2002-2007, but the rate of complex fusion procedures increased 15-fold, from 1.3 to 19.9 per 100,000 Medicare beneficiaries. Complications increased with increasing surgical invasiveness, from 2.3% among patients having decompression alone to 5.6% among those having complex fusions. After adjustment for age, comorbidity, previous spine surgery, and other features, the odds ratio (OR) of life- threatening complications for complex fusion compared with decompression alone was 2.95 (95% confidence interval [CI], 2.50-3.49). A similar pattern was observed for rehospitalization within 30 days, which occurred for 7.8% of patients undergoing decompression and 13.0% having a complex fusion (adjusted OR, 1.94; 95% CI, 1.74-2.17).
Adjusted mean hospital charges for complex fusion procedures were US $80,888 compared with US $23,724 for decompression alone (Deyo, R. JAMA 2010). The MNCM Spine Surgery Measure development workgroup developed patient reported outcome measures for two populations of patients undergoing different lumbar spine procedures, a more complex procedure (lumbar fusion) and a second procedure that represented the most common procedure CPT code 63030 for the most common diagnosis of disc herniation. In 2018, the development workgroup reconvened and redesigned the measure construct to a target-based measure and additionally expanded the denominator for this measure to include all lumbar discectomy laminectomy procedures.
Rationale for measure construct and calculation change:
Target score based on 2016 study in the Spine Journal Fetke, TF et al “What level of pain are patients happy to live with after surgery for lumbar degenerative disorders?” This study compared the Core Outcomes Measures Index (COMI) and symptom well-being questions to two 0 to 10 graphic ratings scales for back and leg pain. Most spine interventions decrease pain but rarely do they totally eliminate it. Reporting of the percent of patients achieving a pain score equivalent to the “acceptable symptom state” may represent a more stringent target for denoting surgical success in the treatment of painful spinal disorders. For disc herniation, this is less than or equal to 2, and for other degenerative pathologies it is less than or equal to 3. The OR benchmark of change (5.0) derived from MNCM data (3 years); the average change in points of patients that did achieve the target of less than or equal to 3.0.
Rationale for the expansion of the denominator and addition of exclusions:
During the original development of this measure, the intent was to have a homogeneous population procedure that represented the most common procedure CPT code 63030 for the most common diagnosis of disc herniation. This strategy did not translate well from ICD-9 to ICD-10 diagnosis codes and the volume of eligible denominator patients dropped significantly. In 2018, the MNCM development workgroup reconvened for measure construct redesign and adopted a broader denominator population; all applicable discectomy laminectomy procedure codes and not limited by a type of diagnosis (includes all). With this decision, the workgroup decided to adopt the same exclusions for the spine fusion population and added exclusions for spine related cancer, acute fracture or infection, neuromuscular, idiopathic or congenital scoliosis.
CLINICAL RECOMMENDATION STATEMENTS:
Journal of Neurosurgery guidelines indicate that there is no evidence that conflicts with the previous recommendations published in the original version of the guideline. This recommendation is for the use of reliable, valid and responsive outcomes instrument to assess functional outcome in lumbar spinal fusion patients. It is recommended that when assessing functional outcome in patients treated for low-back pain due to degenerative disease, a reliable, valid, and responsive outcomes instrument, such as the disease-specific Oswestry Disability Index (ODI), be used (Level II evidence).
MEASURE CALCULATION EXAMPLE:
| Patient | Pre-op VAS | Post-op VAS | Post-op < 3.0? | If No,
(Pre-op minus Post-op) |
If No, Met Improvement Target of > 5.0? | Met Numerator Target? |
| Patient A | 8.5 | 3.5 | No | 5.0 | Yes | Yes |
| Patient B | 9.0 | 2.5 | Yes | na | na | Yes |
| Patient C | 7.0 | 0.5 | Yes | na | na | Yes |
| Patient D | 6.5 | 8.0 | No | -1.5 | No | No |
| Patient E | 8.5 | 2.0 | Yes | na | na | Yes |
| Patient F | 7.5 | 1.5 | Yes | na | na | Yes |
| Patient G | 9.0 | 4.5 | No | 4.5 | No | No |
| Patient H | 5.5 | 7.5 | No | -2.0 | No | No |
| Patient I | 9.0 | 5.0 | No | 4.0 | No | No |
| Patient J | 7.0 | 2.5 | Yes | na | na | Yes |
| Rate | 60% | |||||
| Patient | Pre-op VAS | Post-op VAS | Post-op < 3.0? | If No,
(Pre-op minus Post-op) |
If No, Met Improvement Target of > 5.0? | Met Numerator Target? |
| Patient A | 8.5 | 3.5 | No | 5.0 | Yes | Yes |
| Patient B | 9.0 | 2.5 | Yes | na | na | Yes |
| Patient C | 7.0 | 0.5 | Yes | na | na | Yes |
| Patient D | 6.5 | 8.0 | No | -1.5 | No | No |
| Patient E | 8.5 | 2.0 | Yes | na | na | Yes |
| Patient F | 7.5 | 1.5 | Yes | na | na | Yes |
| Patient G | 9.0 | 4.5 | No | 4.5 | No | No |
| Patient H | 5.5 | 7.5 | No | -2.0 | No | No |
| Patient I | 9.0 | 5.0 | No | 4.0 | No | No |
COPYRIGHT:
© MN Community Measurement, 2023. All rights reserved.
CPT® contained in the Measure specifications is copyright 2004-2023 American Medical Association. ICD-10 is copyright 2023 World Health Organization. All Rights Reserved.
MEASURE TOOL:
Visual Analog Scale (VAS): A visual analog scale is a continuous line indicating the continuum between two states of being.
Visual Analog
Pain Scale
Leg Pain:
How severe is your Leg pain today?
Please place an “X” in a box below the line to indicate how bad you feel your leg pain is today. Please select (“X”) only ONE box. 
The tool must contain the end points of “No Pain” and “Intolerable”. The tool must not display the actual numbers to the patient. It is not acceptable to substitute a numeric rating scale (e.g.; to ask the patient on a scale of one to 10 what number would you use to rate your pain).
Below is the key for MIPS eligible clinicians to utilize in order to convert patient’s “X” to a number for measuring change. Do not use this scale for patient completion. The corresponding numeric value is used for measurement of improvement. The numeric equivalent has 21 possible points from 0 to ten with 0.5 intervals (e.g.; 0, 0.5, 1.0, 1.5, 2.0, 2.5, 3.0). 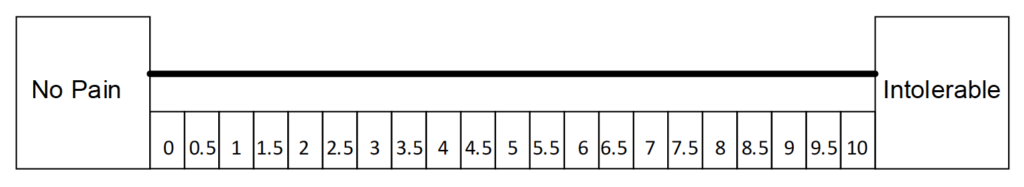
Stay updated with the latest news regarding MACRA and MIPS
The Healthmonix Advisor is a free news source that connects you to the latest in the value-based care industry!